Help Celebrate the First National Biologic Coordinator’s Day
November 1, 2021
 Today, November 1st, is the First National Biologic Coordinator’s Day.
Today, November 1st, is the First National Biologic Coordinator’s Day.
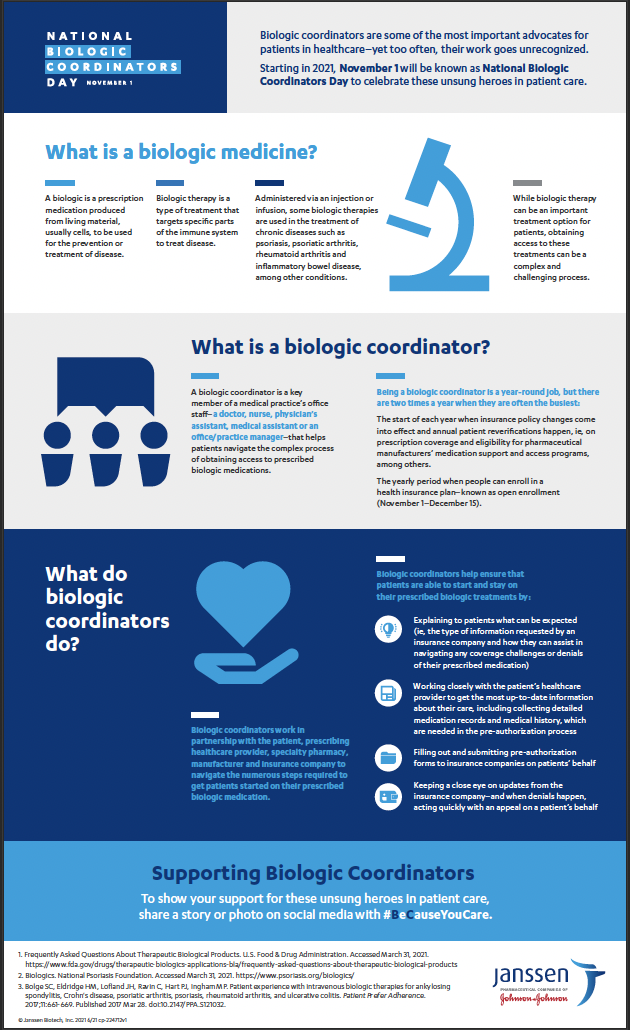
Starting and staying on a prescribed biologic treatment can be a complex process for patients—but it doesn’t always have to be. Thanks to the tireless work of BIOLOGIC COORDINATORS, patients are able to access their prescribed biologic treatments.
A biologic coordinator is a key member of a medical practice’s office staff–a doctor, nurse, physician’s assistant, medical assistant or an office/practice manager–that helps patients navigate the complex process of obtaining access to prescribed biologic medications.
Biologic coordinators are important patient advocates in healthcare—yet too often, their work goes unrecognized.
Show your support today for Biologic Coordinators by using the hashtags #NationalBiologicCoordinatorsDay and/or #BeCauseYouCare!
Learn more about the importance of Biologic Coordinators
by downloading this educational fact sheet: