ASBM Presents at University of the Sciences in Philadelphia
September 15, 2016
On September 15th, 2016, ASBM held an educational forum at the University of the Sciences in Philadelphia (USciences). The program drew 50 attendees comprised of pharmacists, faculty members, pharmacy students.
The program began with an introduction to biosimilars from USciences Associate Professor of Pharmaceutical Sciences Dr. Zhiyu Li. Dr. Li is Director of Undergraduate Pharmacology/Toxicology Program, where he teaches courses on Biomethods in Pharmacology and Toxicology and Biopharmaceutical Proteins.
In order to demonstrate the size and complexity of biologic medicines, Dr. Li described a small-molecule drug (such as aspirin) as being like a bicycle in terms of complexity, whereas a biologic medicine (such as a monoclonal antibody) is more comparable to an airplane.

He then explained that this complexity, and the process by which biologics are grown in living cells, mean that biosimilars can only ever be similar to their reference products- never identical. Even biosimilars grown using an identical sequence as its reference product can result in different end products, likening the two products to twins which look nearly identical yet have different personalities, or the same dish prepared by two different chefs.
ASBM Advisory Board chair Philip Schneider, Associate Dean of the University of Arizona College of Pharmacy, then discussed biosimilars from the perspective of healthcare providers. Dr. Schneider drew upon ASBM surveys of physicians and pharmacists, and more than thirty years’ experience as a professor of pharmacy.
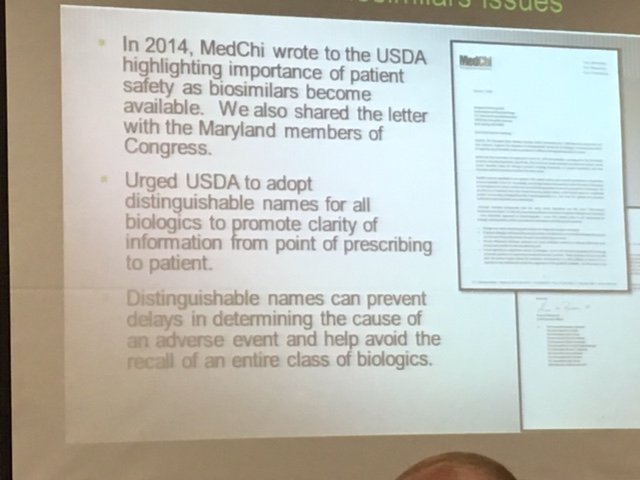
Schneider focused on three main challenges facing policymakers in regard to biosimilars: how they will be named, under what circumstances they may substituted for their reference product, and what information will their labeling include.
Regarding naming, ASBM surveys show that physicians (66%) and pharmacists (68%) overwhelmingly support distinct names for all biologic medicines, including biosimilars. Both the FDA and World Health Organization have proposed accomplishing this by use of a four letter suffix. Of the three biosimilars approved by the FDA, one uses a meaningful suffix derived from its manufacturer’s name-and two use random suffixes.

An informal poll of the audience showed strong support for the meaningful suffix, with most hands raised- by contrast, only one hand was raised in favor of random suffixes. Similarly, an ASBM survey of 400 pharmacists showed 77% support meaningful, memorable suffixes.

![]() Regarding the labeling of biosimilars, Dr. Schneider emphasized the need for informative, transparent labeling that allows physicians and pharmacists to make informed treatment decisions.
Regarding the labeling of biosimilars, Dr. Schneider emphasized the need for informative, transparent labeling that allows physicians and pharmacists to make informed treatment decisions.
Finally, Dr. Schneider discussed how many states- most recently Pennsylvania- allow substitution of “interchangeable” biosimilars- those shown to provide the same results as the reference product without additional risks. The Pennsylvania law, he explained, reflects the importance of good communication between healthcare providers- so that the physician always knows which medicine is dispensed to the patient at the pharmacy, and the patient’s response to a treatment can be accurately assessed. Currently, 24 states and Puerto Rico have enacted similar legislation.

View Dr. Schneider’s presentation here.
The final speaker was Andrew Spiegel, Executive Director of the Global Colon Cancer Association. Mr. Spiegel discussed the tremendous benefits that biosimilars will bring patients- including new treatment choices and reduced healthcare costs- but cautioned that the decision to switch must always remain with the patient and physician, rather than a third party such as a government or insurer. Mr. Spiegel provided several examples of how insurance companies can force patients to switch medicines. This is especially worrisome with biosimilars that are not approved by the FDA as “interchangeable” with their reference product. Many patients with the serious, chronic conditions biologic medicines are used to treat struggle for years and try multiple products before becoming stable. Switching a patient’s medicine for reasons other than health and safety is referred to as Non-Medical Switching, and many patient organizations have raised these concerns when testifying before the FDA.

Additionally, he noted that transparency about how a biosimilar was approved is critical to helping patients make informed choices. For example, the FDA recently approved Inflectra (infiximab-dyyb) for all indications of its reference product for which it applied, despite having demonstrated biosimilarity only in two of the indications- a process called indication extrapolation. By contrast, Health Canada required additional clinical data before granting approval for the extrapolated indications two years later.

View Mr. Spiegel’s presentation here.