October 2021 Newsletter
November 8, 2021
| House Bill Would Distort Treatment Decisions, Undermine Physician-Patient Relationship
The U.S. House of Representatives Committee on Rules has released new language for H.R. 5376 containing a provision that would pay physicians a 33% bonus for prescribing their patient the government-preferred biosimilar.
The bill calls for a “temporary increase in Medicare Part B payments for certain biosimilars,” that would increase the reimbursement to physicians from 6% above average sale price (ASP) to 8%- if they prescribe the biosimilar.
Biosimilars have already achieved significant US market share, around 80% for filgrastim biosimilars, 70% for trastuzumab and bevacizumab biosimilars, and 55% for rituximab biosimilars. As more become available, the increased competition has driven down prices of both biosimilars and innovator biologics.
Despite these successes, supporters of artificially incentivizing biosimilar uptake have continued to insert this provision into several bills in recent years. In July, ASBM sent a letter to Congress opposing this proposal’s inclusion in H.R. 2815. From the letter:
Treatment decisions can and should take into consideration a number of factors, including economic factors such as the affordability of the drug for the patient, but the physician-patient relationship could be seriously undermined when physicians are rewarded financially for choosing one medicine over another. Every patient should be confident that their physician will prescribe the product that is in their best interest, not the one that is the most profitable to the physician personally.
We share the goal of increasing biosimilar uptake and increasing patient access to biologic therapies.
We also firmly believe this proposal is unnecessary, misguided, and potentially harmful. Instead, all products should continue to compete on a level playing field. Advantaging one manufacturer’s product over another not only distorts the treatment-decision making process and undermines the physician-patient relationship, but also undermines the competition-based policies that are currently lowering prices and expanding patient access.
Read ASBM’s full letter here.
|
| Ohio State University College of Pharmacy To Launch Online CE Program
In the coming weeks, the Ohio State University College of Pharmacy will launch a new online Continuing Education (CE) program. Among the first offerings in this program will be a series of presentations related to biologics and biosimilars, sponsored by ASBM. Topics will include a primer on biologics and biosimilars, substitution of biologics and biosimilars, issues with non-medical switching, pharmacovigilance programs and the importance of distinguishable non-proprietary names, the biosimilars market, physician perspectives on biologics and biosimilars, and patient perspectives.
The new CE platform being used at OSU will be available nationwide. With the rapid increase in the number of biologic and biosimilars reaching the market and the advent of interchangeable biosimilars, the need for educational programming for pharmacists is significant.
This program will equip pharmacists with the knowledge needed to play an important role in helping to navigate the increasingly complex challenges associated with the safe and effective use of biologics and the responsible use of limited healthcare resources.
|
| ASBM Presents at World Drug Safety Congress USA 2021
On October 21st, ASBM’s Philip Schneider participated in the World Drug Safety Congress USA 2021, held in Boston, MA. Dr. Schneider led a panel discussion on improving pharmacovigilance programs globally.
Panelists were in general agreement that there is a greater need for improving the quality of adverse drug event reports, particularly in developed countries.
Improvement of biologic pharmacovigilance systems was the topic of a poster abstract presented by Dr. Schneider at the DIA Global Annual Meeting in June 2021. The poster focused on the challenges in accurately identifying biologics in Adverse Drug Reaction (ADR) reports and self-reporting surveys (SRS). For example, in a 2019 analysis of European ADR reports for infliximab in 2018, 35% did not provide a brand name, despite this being required by EU law since 2012.
Another issue discussed in the panel was the need for global harmonization of pharmacovigilance programs so that everyone can benefit from the learnings from these reports. It was agreed that the WHO, which has proposed a global nomenclature standard, would be the logical agency to take the lead in harmonization efforts.
View a video walkthrough of ASBM’s poster on problems with global pharmacovigilance of biologic medicines here.
|
| ASBM Presents at WHO’s 73rd INN Consultation
On October 19th, ASBM participated in the World Health Organization’s 73rd Consultation on International Nonproprietary Names (INN) for Pharmaceutical Substances, held in Geneva, Switzerland. This was the seventeenth INN Consultation in which ASBM has participated.
ASBM was represented by Executive Director Michael Reilly, Esq., and Advisory Board Chair Philip Schneider, MS, FASHP.
“Many published reports, including ASBM’s own surveys of prescribers over several years, show a clear lack of identification of the brand name in ADR reports, especially in the EU in which brand name reporting became a mandatory requirement in 2012.”
“ASBM highlighted that reporting on brand names in ADR reports continues to be inadequate despite widespread recognition of its importance. WHO has identified a lack of a naming standard as a regulatory challenge that undermines the strong pharmacovigilance needed for biologics and biosimilars, and ASBM underlined that the WHO has the ability and the duty to make a global standard available to address this global pharmacovigilance need.”
Since 2013, ASBM has worked extensively on the issue of international harmonization of biologic nomenclature, including holding a series of meetings with FDA, Health Canada, and the WHO on the subject.
Read more about ASBM’s work with the WHO’s INN Group here.
|
| Michael Reilly Op-ed: Forced Biosimilar Switching Would Put Ontario on Wrong Track
On October 5, an op-ed by ASBM Executive Director Michael Reilly ran in several Ontario papers including The Hamilton Spectator, the Welland Tribune, the St. Catharine’s Standard, and the Niagara Falls Review.
The op-ed highlights the concerns with forced-biosimilar-substitution policies
A survey of 403 Canadian specialists found that 73% are uncomfortable with a third party initiating a biologic switch for non-medical reasons (typically the cost), as occurs in the British Columbia and Alberta policies. These findings were affirmed by Quebec’s own government (INESSS) in a May 2020 report which concluded that “Non-medical switching in patients being treated with a reference biologic is generally not accepted by learned societies and the consulted clinicians.”
The Canadian Association of Gastroenterology (CAG) released a paper objecting to the B.C. policy; noting that BC Pharmacare’s substitution policy went against the recommendations of 14 gastroenterology societies throughout Canada and Europe. Many patient advocacy organizations also opposed these policies, including the Gastrointestinal Society and Crohn’s and Colitis Canada.
“It was a very long, difficult 2 1/2 year journey to find [the originally-prescribed] drug. All other drugs failed,” said one B.C. arthritis patient who was forced to switch. “I am shocked and appalled that this government is taking the decision away from physicians and patients, where it belongs.”
The New Brunswick and Quebec announcements cited 15 years of experience with biosimilars in Europe to justify forced switching. However, as the op-ed explains:
Automatic substitution of biologics is almost universally prohibited in Europe. In nearly every European country, physicians are free to choose between multiple products, including the originators, and the payer will reimburse them – resulting in both high biosimilar usage and high savings while preserving patient and physician control of treatment decisions.
Mr. Reilly recently authored similar op-eds in New Brunswick (English) and Quebec (French).
Read ASBM’s recent whitepaper “A Critical Review of Substitution Policy for Biosimilars in Canada.” The paper contrasts the forced-substitution policies of some Canadian provinces with the competition-based approaches which have driven biosimilar uptake in Europe and the U.S.
|
| FDA Finalizes Guidance on Biosimilar Development
In October, the FDA finalized its guidance document “Questions and Answers on Biosimilar Development and the BPCI Act: Guidance for Industry”, addressing additional questions and answers related to biosimilar development. This is the second such revision to the guidance.
The update added five questions, including:
In addition, several questions were withdrawn, while others underwent minor editorial changes.
Learn more about the updated guidance here.
Read the guidance here.
|
| UPCOMING ASBM EVENTS
World Biosimilar Congress Europe 2021 Basel, Switzerland – November 9-11, 2021
16th Biosimilars Congregation 2021 Virtual – December 9, 2021
World Biosimilar Congress USA 2022 San Diego, California – March 9-11, 2022
|
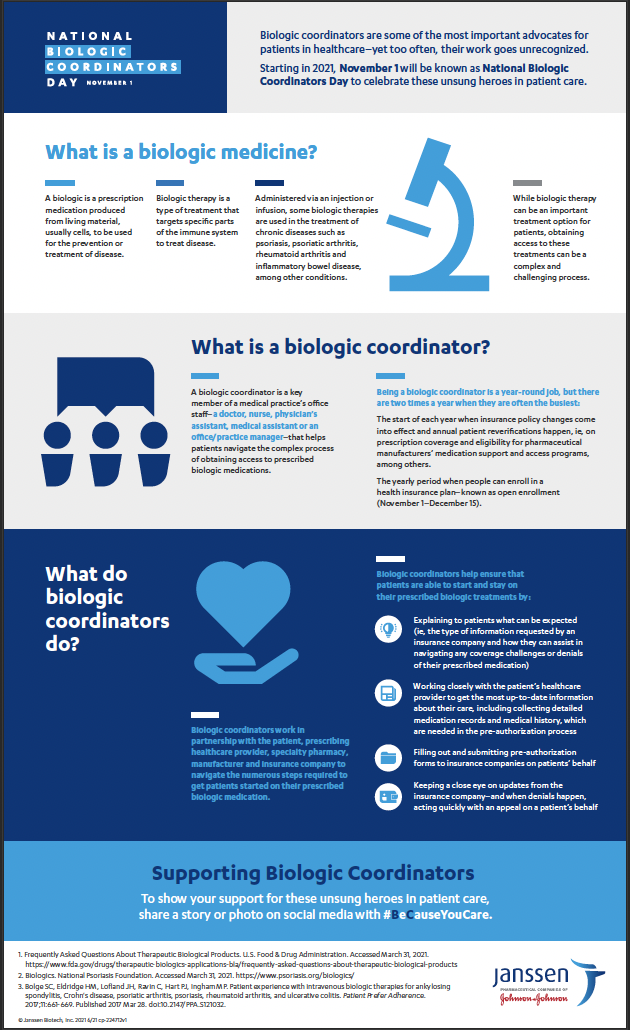
 Today, November 1st, is the First National Biologic Coordinator’s Day.
Today, November 1st, is the First National Biologic Coordinator’s Day.